
Effectiveness of Patient Generated Health Data in Routine Clinical Care
By John Sharp, Senior Manager, Personal Connected Health Alliance of HIMSS
Recently the Office of the National Coordinator for Health IT published the final report on PGHD, titled “Conceptualizing a Data Infrastructure for the Capture, Use, and Sharing of Patient-Generated Health Data in Care Delivery and Research through 2024.” It details the future view of the use of PGHD and "opportunities, challenges, and enabling actions for stakeholder groups." Included in this project are reports on two pilot studies using PGHD from Sutter Health in California and AMITA Health in Illinois.
The Sutter pilot, in partnership with Validic, was designed to demonstrate the flow of data from the patient to the clinician to the researcher. The process of bringing PGHD into a clinical workflow has been a major challenge. Physicians have difficulty managing a stream of raw data from a large panel of patients. Technically, integrating this into the electronic medical record (EMR) has also been a barrier. The solution was to use the following technology pathway:
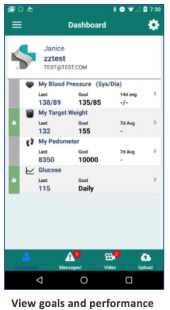
Patients were referred to Mpower using an automated referral workflow already created in the Epic© EHR system. The cohort included patients diagnosed with Type II, non-insulin-dependent diabetes between 21 and 79 years of age whose care is being managed in the primary care setting. The resulting workflow was optimized and is laid out in detail in the ONC report. It stands as a model for future programs integrating PGHD into clinical practice. The patient view included goals and performance, uploading data and receiving nudges and nuggets.
For clinicians, a dashboard enabled a care team to see a continuously updated, risk-stratified view of the population they manage. This dashboard highlighted those patients that required attention, with drill-down into more detailed information on an individual patient.
The AMITA Health pilot demonstration utilized TapCloud across a spectrum of medical conditions to communicate symptoms on a daily basis. Unlike the Sutter Health pilot, AMITA looked at patients with a variety of conditions and collected data about their well-being, pain, symptoms, and medication or treatment adherence. They could also upload photos, for instance, of a post-surgical wound. The basic workflow included:
Patients received personalized care plans and medication reminders and tracked adherence to those plans and medications. They could also communicate with clinicians through the app. One of the unique features of the apps is the “symptom cloud,” a user-friendly touchscreen.
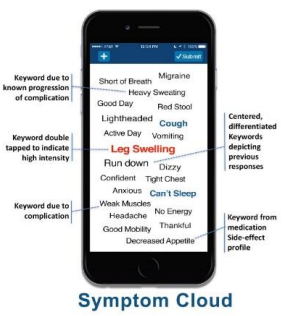
Patients and providers each had their customized dashboards, including provided symptom tracking and alerts.
The comprehensive review of workflow is included in the ONC report.
In summary, these pilot projects provide three key components to advance the collection and use of PGHD:
- A method for transferring data securely from the patient to the provider EMR.
- Actionable user interfaces for clinicians to monitor patients.
- Patient engagement through user-friendly technology.
Looking forward to the clinical outcomes of these pilots to demonstrate the effectiveness of these monitoring activities and any potential cost savings from these programs.
PGHD and this report will be discussed in the Innovation Leaders Program at HIMSS18.




