Strengthening Evidence-Based Care in Digital and Telehealth
By John Sharp, Senior Manager, Personal Connected Health Alliance
While hype and enthusiasm for digital health technologies and telehealth seem boundless, solid evidence for supporting care decisions are harder to come by. Two publications now clarify the evidence and propose a way forward.
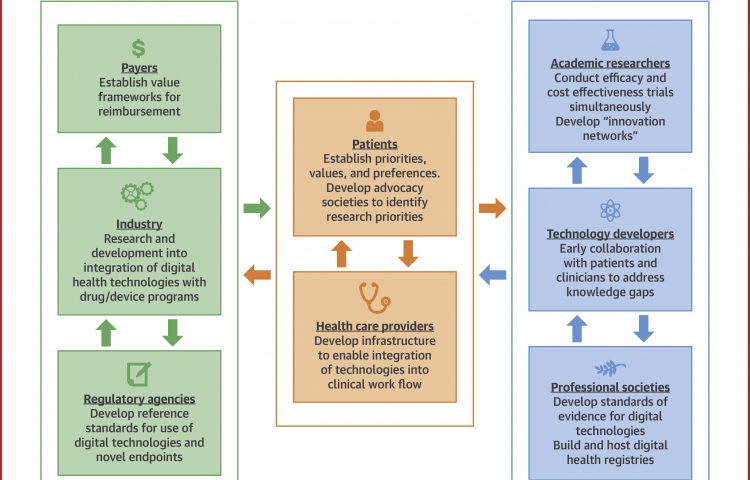
First, the Journal of the American College of Cardiology published a review article that is the result of a think tank meeting convened in late 2017. The article, Using Digital Health Technology to Better Generate Evidence and Deliver Evidence-Based Care, describes the three aims of this meeting: understanding the current landscape, identifying barriers to development and adoption, and potential solutions. They examined solutions from all stakeholders who participated including regulatory, industry, agencies, providers and even professional societies, such as, the ACC. The authors addressed several use cases including digital health in diagnostics, disease management and decision support, research recruitment, informed consent, and digital clinical study endpoints (aka, digital biomarkers).
The challenges are many: quality of data and interoperability, questionable improvements in productivity, privacy and security. Specific recommendations provide a future direction: development of innovation networks, models of which already exist;, better collaboration with regulators, such as, through the U.S. Food and Drug Administration (FDA) Pre-Cert program; expanding the role of professional societies; and more public-private partnerships.
The second piece of evidence is from AHRQ (Agency for Healthcare Research and Quality), a draft systematic review on Telehealth for Acute and Chronic Care Consultations. This 140-page report focuses on tele-ICU, telehealth for inpatient care and telehealth consultations for outpatient care. Categorizing the strength of evidence from high to insufficient, the authors found that remote ICU consultations likely reduce ICU mortality. They also found less evidence that inpatient consultations will reduce length of stay and costs, and no difference for telestroke consultations. The group also recommended that studies include information on potential harms and better measurement of cost outcomes.
Researchers are encouraged to design more robust studies, include a broad range of stakeholders, study costs and potential harms as well as medical outcomes to move evidence-based care forward.




